VA Asthma & Respiratory Rating Criteria Explained
When VA grants service connection for asthma or another respiratory condition, it assigns a disability rating based on severity measured through pulmonary function testing, medication use, frequency of attacks, and overall impact on daily life. These ratings determine a veteran’s monthly compensation and additional benefits. Because asthma and respiratory disorders often fluctuate or worsen over time, it is essential that a veteran’s claim or appeal clearly documents the full extent of their symptoms.
VA rates asthma and most respiratory conditions under 38 C.F.R. § 4.97 (Diagnostic Code 6602) using pulmonary function tests (PFTs), medication use, frequency of exacerbations, and hospitalizations. Ratings commonly fall at 10, 30, 60, or 100 percent, depending on severity.
A veteran’s C&P exam, pulmonary testing, treatment notes, and lay statements are all critical forms of evidence when seeking higher ratings for asthma or related disorders.
Veterans with severe respiratory conditions may qualify for additional benefits, including Total Disability Based on Individual Unemployability (TDIU) or Special Monthly Compensation (SMC).
Bottom Line Up Front:
How Does VA Assign Ratings for Asthma and Respiratory Disorders?
VA evaluates respiratory disabilities using a combination of objective medical testing and documented symptoms. The most common evidence sources include:
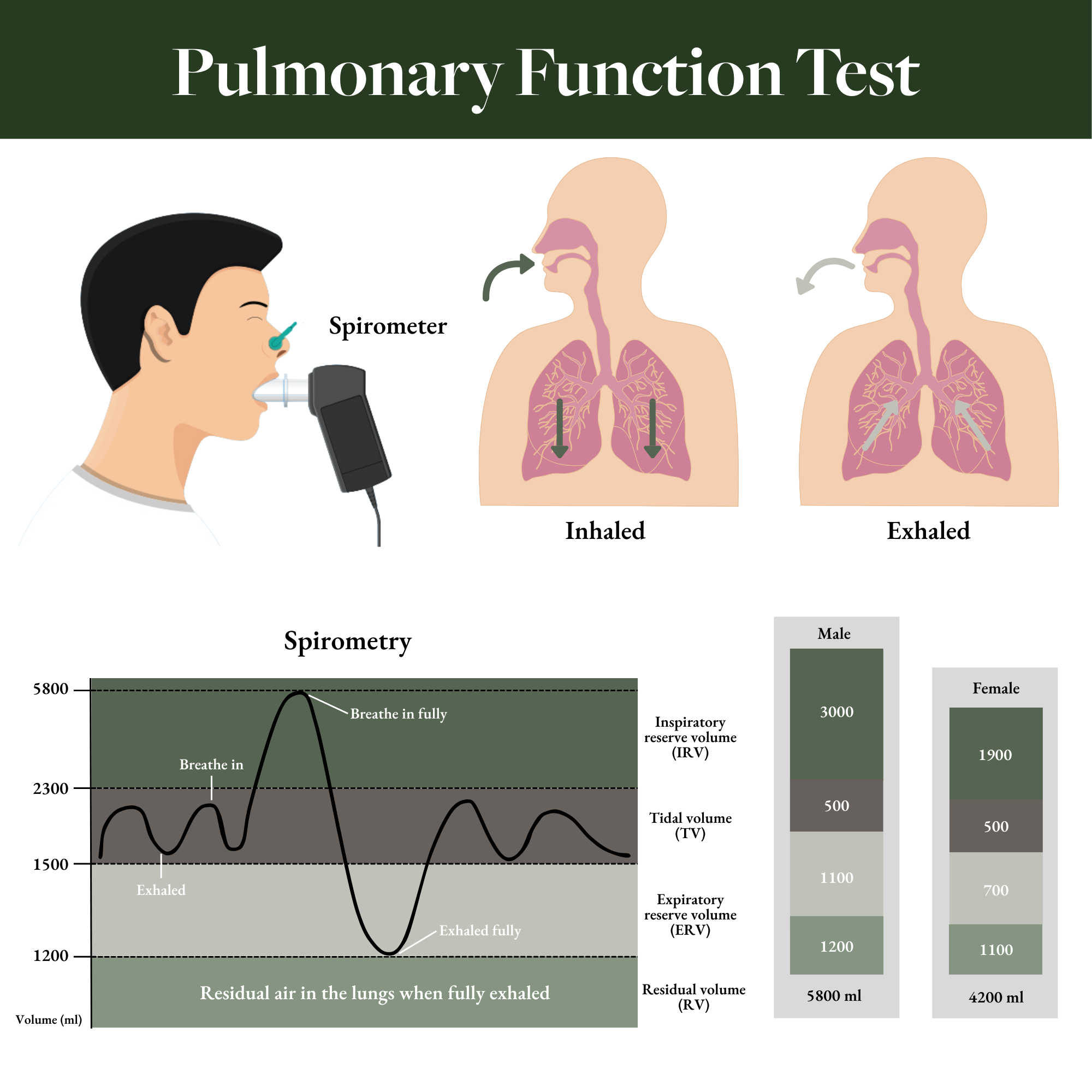
C&P Exams and Pulmonary Function Tests (PFTs)
For asthma, chronic bronchitis, COPD, and restrictive lung disorders, the C&P examiner often conducts or references:
FEV-1 (Forced Expiratory Volume in one second)
FEV-1/FVC ratio
DLCO (Diffusion Capacity)
Use and frequency of systemic corticosteroids
Frequency of asthma attacks requiring physician visits
Missed work, ER visits, or hospitalizations
PFT results are central to respiratory ratings, but they are not the only factor. VA must consider additional symptoms such as:
Dyspnea (difficulty breathing)
Wheezing
Chronic cough
Use of inhalers or nebulizers
Frequency of exacerbations requiring medical intervention
VA examiners complete a Respiratory Conditions Disability Benefits Questionnaire (DBQ) to standardize the evaluation.
Lay Evidence
Lay statements can be extremely useful in respiratory claims. Veterans and witnesses can describe:
How often asthma attacks occur
Whether symptoms limit exertion, exercise, or work
Frequency of nighttime symptoms
The impact of environmental triggers (cold air, allergens, smoke)
The veteran’s need to stop activities due to shortness of breath
Asthma symptoms fluctuate, and PFT results taken on a “good day” do not necessarily reflect a veteran’s usual functioning. Lay testimony helps bridge that gap.
Private Medical Records
Pulmonologists or allergy specialists frequently have longitudinal records that VA examiners do not. These may include:
Long-term inhaled or systemic corticosteroid use
Hospitalizations for asthma attacks
Serial PFTs demonstrating worsening
Bronchitis or pneumonia flare-ups
Sleep disturbance due to nighttime wheezing
Providing complete private records can make or break an asthma or respiratory claim. Veterans may also obtain private nexus opinions to link asthma or secondary respiratory issues (e.g., chronic sinusitis, allergies, sleep apnea) to service.
How VA Rates Asthma & Related Respiratory Conditions (38 C.F.R. § 4.97)
VA uses diagnostic code 6602 for asthma, but related conditions such as chronic bronchitis, COPD, interstitial lung disease, and restrictive lung disorders have similar rating principles.
100 Percent Rating for Asthma
A 100 percent rating reflects pronounced respiratory impairment, often including:
FEV-1 less than 40% predicted
FEV-1/FVC less than 40%
More than one asthma attack per week with respiratory failure
Near-constant inhalation or oral bronchodilator therapy
Frequent systemic corticosteroid courses
Episodes requiring hospitalization
A veteran at 100 percent typically cannot sustain physical exertion and may struggle with daily tasks due to severe breathing limitations.
60 Percent Rating for Asthma
A 60 percent rating is warranted when the veteran has:
FEV-1 of 40–55% predicted
FEV-1/FVC of 40–55%
At least three systemic corticosteroid courses per year
Frequent medical intervention for exacerbation
This level generally reflects moderate-to-severe impairment with significant restrictions on work activity.
30 Percent Rating for Asthma
A 30 percent disability rating is assigned for:
FEV-1 of 56–70% predicted
FEV-1/FVC of 56–70%
Daily inhalational or bronchodilator therapy
Inhaled anti-inflammatory medication (e.g., corticosteroid inhalers)
** Most veterans with persistent asthma fall within this category
10 Percent Rating for Asthma
A 10 percent rating typically reflects intermittent or mild asthma, including:
FEV-1 of 71–80% predicted
FEV-1/FVC of 71–80%
Intermittent inhalational bronchodilator therapy
Symptoms may flare with exercise or environmental triggers but do not consistently interfere with occupational or social functioning.
0 Percent (“Non-Compensable”) Respiratory Ratings
A 0 percent rating is assigned when asthma is formally diagnosed but:
PFTs are normal
Symptoms do not require continuous medication
The condition does not impair work or daily activity
Even with a 0 percent rating, service connection is valuable because:
The veteran can file for an increase if symptoms worsen
VA healthcare access and priority status may improve
Additional Factors Affecting Respiratory Ratings
Multiple Respiratory Diagnoses
Many respiratory conditions share symptoms (wheezing, shortness of breath, cough), so VA often assigns one combined rating to avoid pyramiding. For example, asthma with chronic bronchitis may be rated under the single predominant diagnosis.
Respiratory Conditions and TDIU
Asthma and related lung conditions can severely impair a veteran’s ability to work, especially in jobs requiring:
Physical labor
Exposure to fumes, dust, cold air, or chemicals
High levels of exertion
Veterans rated at 60 percent for a single condition (or 70 percent combined) may be eligible for Total Disability Based on Individual Unemployability (TDIU), providing compensation at the 100 percent rate.
Special Monthly Compensation (SMC)
Respiratory disorders rarely qualify for SMC directly unless they:
Result in housebound status
Cause significant secondary complications
However, severe asthma combined with other service-connected disabilities may create eligibility.
How to Appeal or Increase a VA Respiratory Rating
Veterans may want to appeal or request an increase if:
VA denied service connection
VA underrated their asthma
PFT results worsened over time
They developed a secondary condition (e.g., sinusitis, allergies, GERD, sleep apnea)
They believe VA overlooked medication use or steroid courses
Appeals can be filed through:
Higher-Level Review
Supplemental Claim with new and relevant evidence
Board Appeal
Because respiratory ratings rely heavily on technical medical data, many veterans benefit from professional representation during appeals.
Denied or Underrated for VA Asthma or Respiratory Disability? Call Greene & Marusak LLC
Respiratory claims are complex and often require detailed medical evidence, expert opinions, and strategic argument. If VA denied or underrated your asthma or respiratory condition, Greene & Marusak LLC can help.
Contact us for a free case evaluation today to speak with an experienced VA-accredited claims agent or attorney.