VA Rating Criteria for PTSD & Mental Disorders Explained
When VA grants service connection for post-traumatic stress disorder (PTSD) or another mental health disability, it assigns a disability rating based on the frequency and severity of a veteran’s occupational and social impairment. These ratings determine a Veteran’s monthly compensation and additional benefits.
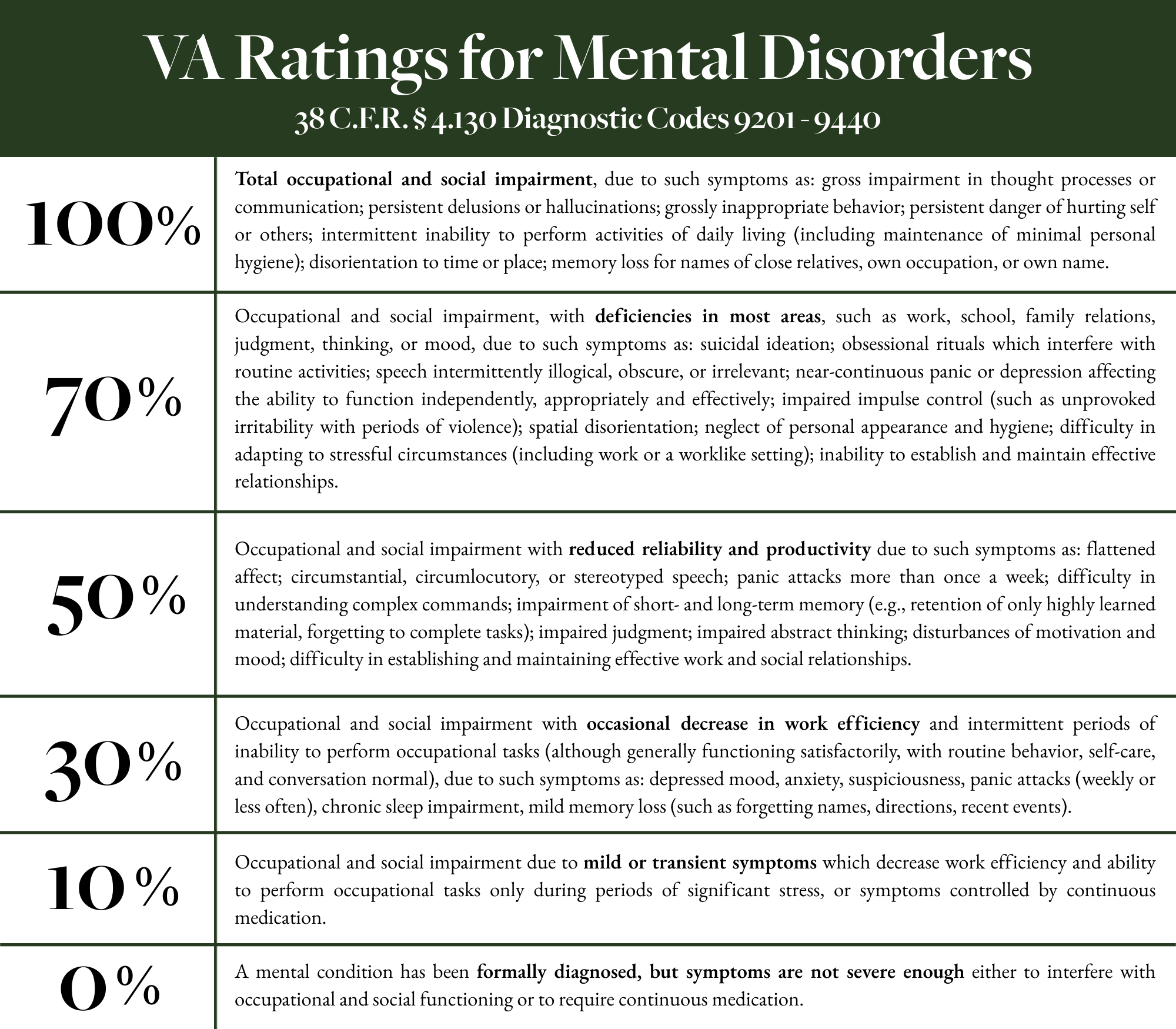
VA rates PTSD and other mental disorders under 38 C.F.R. §4.130, covering diagnostic codes 9201-9440. Ratings commonly fall at 10, 30, 50, 70, or 100 percent, depending on the occupational and social impairment.
A veteran’s C&P exam, treatment records, lay statements, and buddy statements are all critical evidence VA relies on in assigning a rating for PTSD or other mental disorders.
Veterans whose PTSD or other mental disorders impact their ability to work may qualify for a Total Disability Based on Individual Unemployability (TDIU)
Bottom Line Up Front:
How Does VA Assign Ratings for PTSD & Mental Disorders?
VA evaluates psychiatric disabilities using a combination of examinations, treatment records, and a veteran’s reports of their symptoms.
The most common evidence sources include:
C&P Exams
For PTSD and other mental health conditions, VA relies heavily on Compensation & Pension (C&P) examinations, which are typically completed using standardized Disability Benefits Questionnaires (DBQs). Most psychiatric conditions, including PTSD, are evaluated using the Mental Disorders DBQ, while conditions such as anorexia nervosa or bulimia nervosa may be evaluated using the Eating Disorders DBQ, depending on the diagnosis.
During the exam, the examiner confirms a current diagnosis under DSM criteria, reviews the veteran’s claims file, and evaluates the level of occupational and social impairment consistent with VA’s rating criteria under 38 C.F.R. § 4.130. The examiner documents the veteran’s relevant social, marital, family, occupational, educational, mental health, legal, behavioral, and substance use history, as applicable.
Using the DBQ, the examiner identifies the veteran’s symptoms based on both the evidence of record and the clinical interview, and explains how those symptoms impact daily functioning and the ability to work. If raised by the record, the examiner may also address the veteran’s competency to manage VA funds and include additional remarks to clarify symptom severity or functional limitations.
VA and/or Private Treatment Records
When assessing the frequency and severity of a veteran’s mental health disability, VA is required to review all pertinent evidence of record, rather than rely solely on a VA examination. VA and private mental health treatment records often provide a more accurate and detailed picture of a veteran’s day-to-day functioning than a one-time C&P exam.
Frequency and consistency of mental health treatment
Reports of suicidal or homicidal ideation
Ongoing stressors or conflicts involving family, friends, or work
Clinical observations that provide a more complete picture of the severity and persistence of the mental health condition
Examples of useful evidence found in treatment records include, but are not limited to:
These records can document the progression of symptoms over time, response to treatment, and the real-world impact of the condition on the veteran’s personal, social, and occupational life.
Lay & Buddy Statements
Lay and buddy statements are a powerful form of evidence in the VA disability compensation process, particularly for mental health claims. Lay statements allow the veteran to describe their symptoms and functional limitations based on firsthand experience. These statements are especially important because many veterans unintentionally under-report symptoms during VA examinations, often due to discomfort discussing personal or traumatic experiences with an unfamiliar examiner.
Without a full and accurate description of symptoms, VA may underrate a veteran’s mental health condition. Lay statements help fill this gap by explaining how symptoms affect daily life, relationships, and the ability to function over time—information that may not be fully captured during a single C&P exam.
Buddy statements provide additional supporting evidence from people who know the veteran, such as family members, friends, or fellow service members. These statements can describe observable changes in behavior, mood, and functioning, as well as corroborate in-service stressors or ongoing mental health symptoms when VA has difficulty verifying them through official records.
Together, lay and buddy statements help provide VA with a more complete and accurate picture of the veteran’s mental health disability and its real-world impact.
How VA Rates PTSD & Other Mental Disorders (38 C.F.R. § 4.130)
VA evaluates PTSD under Diagnostic Code 9411, but most mental health conditions—including depression, anxiety disorders, bipolar disorder, and eating disorders—are rated under the General Rating Formula for Mental Disorders, which applies to diagnostic codes 9201–9440.
Rather than focusing on a single symptom, VA assigns ratings based on the overall level of occupational and social impairment caused by the condition. The symptoms listed at each rating level are examples, not requirements. A veteran does not need to show every symptom listed to qualify for a particular rating.
100 Percent Rating
A 100 percent rating is assigned when the mental health condition results in total occupational and social impairment. This level reflects a veteran who is essentially unable to function in a work or social environment due to the severity of their symptoms.
Examples of symptoms associated with this level include:
Gross impairment in thought processes or communication
Persistent delusions or hallucinations
Grossly inappropriate behavior
Persistent danger of hurting self or others
Inability to perform activities of daily living, including maintaining basic personal hygiene
Disorientation to time or place
Severe memory loss, such as forgetting names of close relatives or one’s own occupation
This rating is reserved for the most severe cases and often overlaps with entitlement to TDIU when total impairment is shown.
70 Percent Rating
A 70 percent rating is warranted when symptoms cause occupational and social impairment with deficiencies in most areas, such as work, school, family relations, judgment, thinking, or mood.
Suicidal ideation
Obsessional rituals that interfere with routine activities
Illogical, obscure, or irrelevant speech
Near-continuous panic or depression affecting independent functioning
Impaired impulse control, including anger or periods of violence
Neglect of personal appearance or hygiene
Difficulty adapting to stressful circumstances, including work settings
Inability to establish and maintain effective relationships
This level often reflects serious, ongoing symptoms that significantly interfere with daily life and employment, such as:
Veterans rated at 70 percent frequently struggle to maintain employment and may also qualify for TDIU.
50 Percent Rating
A 50 percent rating applies when the condition causes occupational and social impairment with reduced reliability and productivity. Veterans at this level are sometimes able to work but experience significant difficulty maintaining consistent performance or stable relationships.
Flattened affect
Panic attacks more than once per week
Difficulty understanding complex commands
Memory impairment affecting work tasks
Impaired judgment or abstract thinking
Disturbances of motivation and mood
Difficulty establishing and maintaining effective work and social relationships
Common symptoms at this level include:
This rating often reflects noticeable functional decline compared to pre-service or earlier functioning.
30 Percent Rating
A 30 percent rating is assigned when symptoms result in occasional decreases in work efficiency with intermittent periods of inability to perform occupational tasks, but overall functioning remains generally satisfactory.
Depressed mood or anxiety
Suspiciousness
Panic attacks occurring weekly or less often
Chronic sleep impairment
Mild memory loss
Examples include:
Veterans at this level are usually able to maintain employment but experience periodic interference from their symptoms.
10 Percent Rating
A 10 percent rating applies when symptoms are mild or transient and only interfere with work efficiency during periods of significant stress, or when symptoms are well controlled by continuous medication.
This level reflects minimal functional impairment.
Multiple Mental Health Diagnoses
Many mental health conditions share overlapping symptoms, such as depression, anxiety, sleep impairment, irritability, and difficulty concentrating. To avoid pyramiding, VA generally assigns one combined rating under the General Rating Formula for Mental Disorders, even when a veteran has multiple diagnosed conditions (for example, PTSD with major depressive disorder or anxiety disorder).
In these cases, VA is required to evaluate the overall level of occupational and social impairment, rather than attempt to separate symptoms by diagnosis. The focus is on how the veteran functions as a whole, not on the number of mental health diagnoses.
Mental Disorders, TDIU, & SMC
Concentration, memory, and task completion
Attendance, reliability, or pace
Interactions with supervisors, coworkers, or the public
Ability to adapt to stress or changes in a work environment
Mental health conditions can significantly impair a veteran’s ability to maintain substantially gainful employment, particularly when symptoms affect:
Mental Disorders and TDIU
Veterans with a single mental health rating of 60 percent or higher, or a combined rating of 70 percent with one condition rated at least 40 percent, may be eligible for Total Disability Based on Individual Unemployability (TDIU), which pays compensation at the 100 percent rate even when schedular criteria are not met.
Results in the need for regular aid and attendance
Causes the Veteran to be substantially confined to the home
Combines with other service-connected disabilities to meet SMC criteria
Mental disorders do not often qualify for Special Monthly Compensation (SMC) on their own. However, SMC may be warranted when a mental health condition:
Special Monthly Compensation (SMC)
Severe psychiatric symptoms, particularly when accompanied by physical disabilities, may support entitlement to SMC in certain cases.
How to Appeal or Increase a Mental Disorder Rating
Veterans may want to appeal or request an increased rating if:
VA denied service connection for a mental health condition
VA underrated the severity of PTSD or another mental disorder
Symptoms have worsened over time or increased in frequency
The condition has begun to interfere more significantly with employment or daily functioning
VA failed to properly consider treatment records, lay statements, or favorable medical evidence
Higher-Level Review
Supplemental Claim with new and relevant evidence
Board Appeal
Appeals can be filed through:
Because mental disorder ratings rely heavily on subjective evidence, many veterans benefit from professional representation during appeals.
PTSD and other mental disorder claims are complex and often require detailed medical evidence, expert opinions, and strategic argument. If VA denied or underrated your PTSD or other mental disorder, Greene & Marusak LLC can help.
Denied or Underrated for PTSD or Mental Disorder Disability? Call Greene & Marusak LLC
Contact us for a free case evaluation today to speak with an experienced VA-accredited claims agent or attorney!